Research
Jul 29, 2024
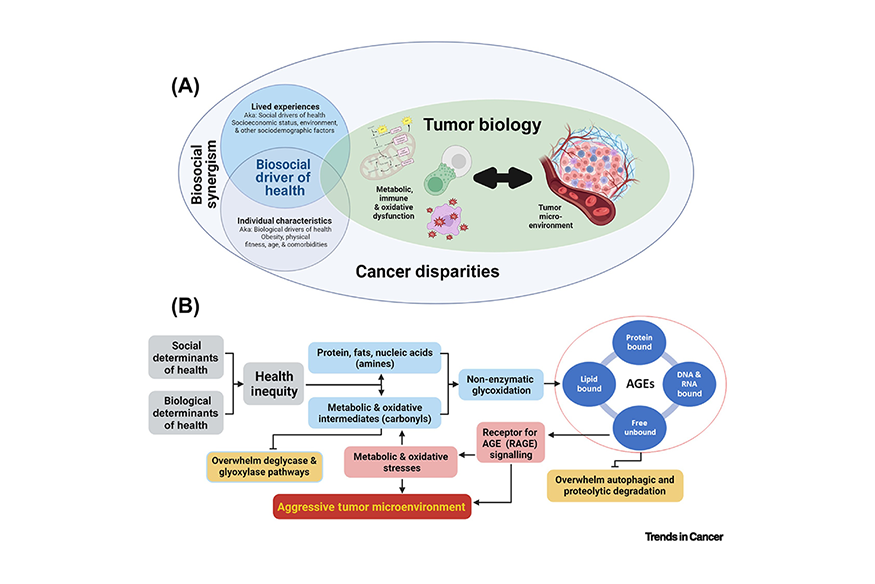 This figure demonstrates how biosocial synergism impacts cancer disparities. (Illustration published in Trends in Cancer)
This figure demonstrates how biosocial synergism impacts cancer disparities. (Illustration published in Trends in Cancer)
Scientists at VCU Massey Comprehensive Cancer Center have coined a new term — “biosocial determinants of health” — to define the interaction of biological, environmental and social drivers that influence cancer risk, incidence and disparities.
Through a new paper published in Trends in Cancer, study authors are calling for new, more comprehensive research that looks at biosocial determinants of health — both social and biological factors together — to better understand and more effectively eradicate a variety of cancer inequities.
The authors include Victoria Findlay, Ph.D., co-leader of the Cancer Prevention and Control research program at Massey and associate professor in the Department of Surgery at the VCU School of Medicine; David Turner, Ph.D., interim associate co-director of Community Outreach and Engagement at Massey, as well as vice chair of Research and Innovation in the Department of Surgery at the VCU School of Medicine; and Robert A. Winn, M.D., director and Lipman Chair in Oncology at Massey.
“Understanding and addressing the role of biosocial determinants of health in cancer progression is a vital step toward reducing disparities and improving health outcomes for all,” said Findlay. “One thing remains clear, assessing social or biological determinants of health in isolation will not answer our critical questions regarding the root cause of enduring cancer disparities.”
Cancer disparities — differences in cancer rates and outcomes among different groups — are influenced by both social and biological factors. Social determinants, or drivers, of health include things such as income, education and one’s environment. In contrast, biological determinants of health include genetics, ancestry, physical activity and personal health conditions, among others. Although previous efforts to address these issues individually have resulted in an overall improvement in cancer outcomes, some disparities remain or have even worsened.
The study authors have been at the forefront of exploring the complex relationship of lifestyle factors and biology, one primary example being the accumulation of harmful compounds in the body called advanced glycation end products (AGEs). These compounds are formed when sugar combines with fat, protein and other genetic materials. Diet, lack of physical activity and other health conditions contribute to an increase in AGE formation.
Extensive research by Findlay and Turner demonstrates that the accumulation of AGEs is directly linked to increased metabolic stress, oxidative stress and inflammation, laying the cellular groundwork for the development of chronic diseases, including cancer.
“If you have a really unhealthy lifestyle, you might have a chronological age of 30 but the biological age of your tissues could be 50,” said Turner. “We’ve shown in a lot of our models that if you consume a lot of AGEs, it makes your tumors grow four to five times quicker.”
The intersection of dietary habits, socioeconomic status and environmental factors plays a crucial role in cancer disparities and exposure to AGEs. For instance, those who live in rural areas with less access to effective medical care tend to be less versed in science and healthy habits, which can increase their exposure to AGEs. Understanding how social and biological factors cooperate can help researchers develop better strategies to reduce cancer disparities.
Findlay and Turner are currently looking into how AGEs are formed, where they come from, how they cause tumors to grow, prevention strategies and methods to mitigate their negative health impacts, with the ultimate goal of creating interventional strategies and informing the community.
“Education about our science is the most important thing. It doesn’t matter what we do because if we can’t get it out into the community, it’s never going to be adopted as a lifestyle change,” Findlay said.
This study was funded by the National Cancer Institute (P20CA264067, P20CA252717, R01CA245143, R01CA259415 and R21CA258139), the National Institute on Minority Health and Health Disparities (R01MD014839) and Stand Up To Cancer (SU2C6228).
Written by: Jessica Desamero, Shaniqua Hayes, Madison Ward and Michael Wong (Walter Lawrence scholars at Massey)
Research
Undergraduate student embraces the chance to write her own story in cancer researchAug 30, 2024
Research, Clinical, Technology
VCU team has designs on a game-changer in women’s cancer treatmentAug 29, 2024
Research, Center News & Funding
With new grant funding, researcher hopes to take down multiple drivers of lung cancer with a single strikeAug 08, 2024

Treatments in clinical trials may be more effective or have fewer side effects than the treatments that are currently available. With more than 200 studies for multiple types of cancers and cancer prevention, Massey supports a wide array of clinical trials.

Massey supports hundreds of top cancer specialists serving the needs of our patients. Massey’s medical team provides a wealth of expertise in cancer diagnosis, treatment, prevention and symptom management.